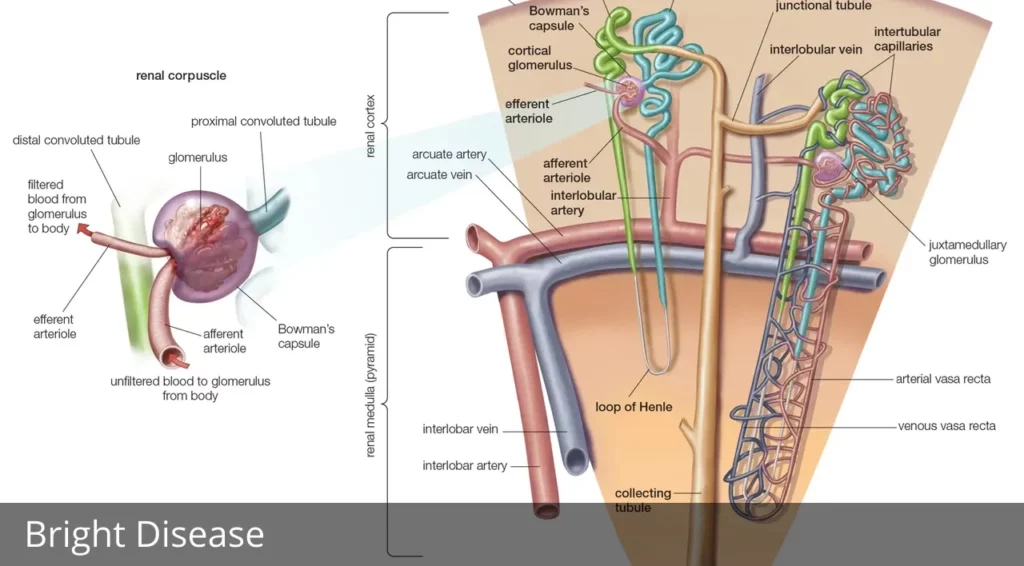
Bright disease: Inflammation of the glomeruli and nephrons, two kidney structures responsible for urine production, characterizes the Bright disease, also known as glomerulonephritis or nephritis. Bowman’s capsule encases the glomeruli, which are circular collections of capillaries (microscopic blood vessels). The other end of Bowman’s capsule attaches to a long tubule.
A nephron is a capsule and the tubule that it connects to. Glomerulonephritis is an inflammation of the kidney’s filtering units (glomeruli), filtering units (nephrons), and interstitial tissues. Diseases with similar symptoms were defined as “Bright Disease” after the British doctor Richard Bright first documented them in the 1820s and ’30s. Due to their intricacy, the diseases described by Bright have eventually been renamed glomerulonephritis (or nephritis).
Diseases like systemic lupus erythematosus and inflammation of the arteries can both damage the glomeruli and lead to glomerulonephritis (e.g., high blood pressure [hypertension] or diabetic nephropathy). Streptococcal infections, such as those that cause strep throat, can also cause glomerulonephritis. However, in certain instances, the root of the problem remains elusive.
A single episode of glomerulonephritis is possible, but recurrence is also possible. Acute, subacute, and chronic describe the escalating severity of the condition. Acute glomerulonephritis causes several symptoms, including acute inflammation, renal (kidney) failure, edema, high blood pressure, and excruciating back pain.
Although most people fully recover from acute glomerulonephritis, even mild infections can cause permanent kidney damage and progress the disease into the subacute and chronic stages when symptoms persist even after the acute phase has passed. The kidneys are enlarged, the capsule enclosing each kidney is taut and strained, the surface is smooth and grey, and there are typically many tiny hemorrhages from the capillaries in the acute stage of the disease.
The glomeruli and nephrons cluster as a whole enlarge. Subacute glomerulonephritis does not necessarily follow acute attacks; if it does emerge, however, it has frequently been preceded by an acute episode several months or years earlier. The kidney grows greatly enlarged, the surface is smooth and pale, and the inside tissue is darker than usual.
The buildup of fat (lipid) droplets on the skin’s surface and the resulting lack of oxygen supply is to blame for the kidneys’ pallor. An accumulation of character (epithelial) cells, erythrocytes, and mineral crystals occurs in Bowman’s capsules. Damage to the nephron tubules is the first sign of kidney failure.
Typically, the kidneys would excrete just a certain amount of blood protein, but when they start to break down, this amount is discharged in excess in the urine. When red blood cells are squeezed through narrowed glomeruli, they become damaged and die off, leading to anemia.
A few people who appear to have never had kidney illness have been found to have chronic glomerulonephritis after surviving the first two phases. The kidney has been almost entirely replaced by scar tissue at this point. The surface is rough, and the object is small. Because the blood cannot be filtered out of waste items, high concentrations of nitrogenous compounds in the blood induce the disease known as uremia.
Richard Bright, British physician was the first to describe edema and proteinuria as the primary clinical symptoms of kidney disorders known as Bright’s disease/nephritis in his book Reports of Medical Cases (1827)#NephHistory #NephTwitter #NephTrivia pic.twitter.com/4zpyDTMDvK
— ISN Education (@ISNeducation) January 14, 2021
Treatment of all kinds of glomerulonephritis is generally oriented toward controlling high blood pressure using antihypertensive medicines, diuretics, and changes in diet, including fluid restriction and decreased salt intake. In some cases, anti-inflammatory medications effectively alleviate the patient’s symptoms. Uremia treatment options include dialysis.
What Treatments Are Available For Bright Disease?
Treatment options vary on the type of Bright disease you’re experiencing and its source.
One treatment is to reduce excessive blood pressure, especially if that’s the underlying cause of the Bright Disease. Blood pressure may be tough to control when your kidneys aren’t performing correctly. If this is the case, your doctor may prescribe blood pressure drugs, including angiotensin-converting enzyme inhibitors, or ACE inhibitors, such as:
- captopril
- lisinopril (Zestril)
- perindopril (Aceon)
Your doctor may also prescribe angiotensin receptor blockers, or ARBs, such as:
- losartan (Cozaar)
- irbesartan (Avapro)
- valsartan (Diovan)
Corticosteroids may also be utilized if your immune system is targeting your kidneys. They reduce the immunological response. Another way to minimize immune-triggered inflammation is plasmapheresis. This treatment takes the fluid part of your blood, called plasma, and replaces it with intravenous fluids or donated plasma that contains no antibodies.
For chronic GN, you’ll need to lower the quantity of protein, salt, and potassium in your diet. Additionally, you must watch how much fluids you ingest. Calcium supplements may be prescribed, and you may need to take diuretics to minimize edema. Check with your general practitioner or kidney specialist for suggestions about diet restrictions or supplements.
They can set you up with a medical dietician to assist you with your choices. If your condition develops advanced and you suffer renal failure, you may need to have dialysis. When undergoing this process, your blood will be filtered by a machine. You may require a kidney transplant in the future.